Superinfections can pose serious challenges in medical treatments, complicating patient care and recovery. Understanding what event triggers the development of a superinfection is crucial in avoiding further health complications. In this blog, we delve into the intricate connections between the occurrence of specific events and the onset of superinfections. By exploring the underlying causes and risk factors, we aim to shed light on this complex phenomenon. Join us as we unravel the mystery behind the triggers that pave the way for superinfections to emerge, providing valuable insights for healthcare professionals and patients alike.
The Rise of Antibiotic Resistance
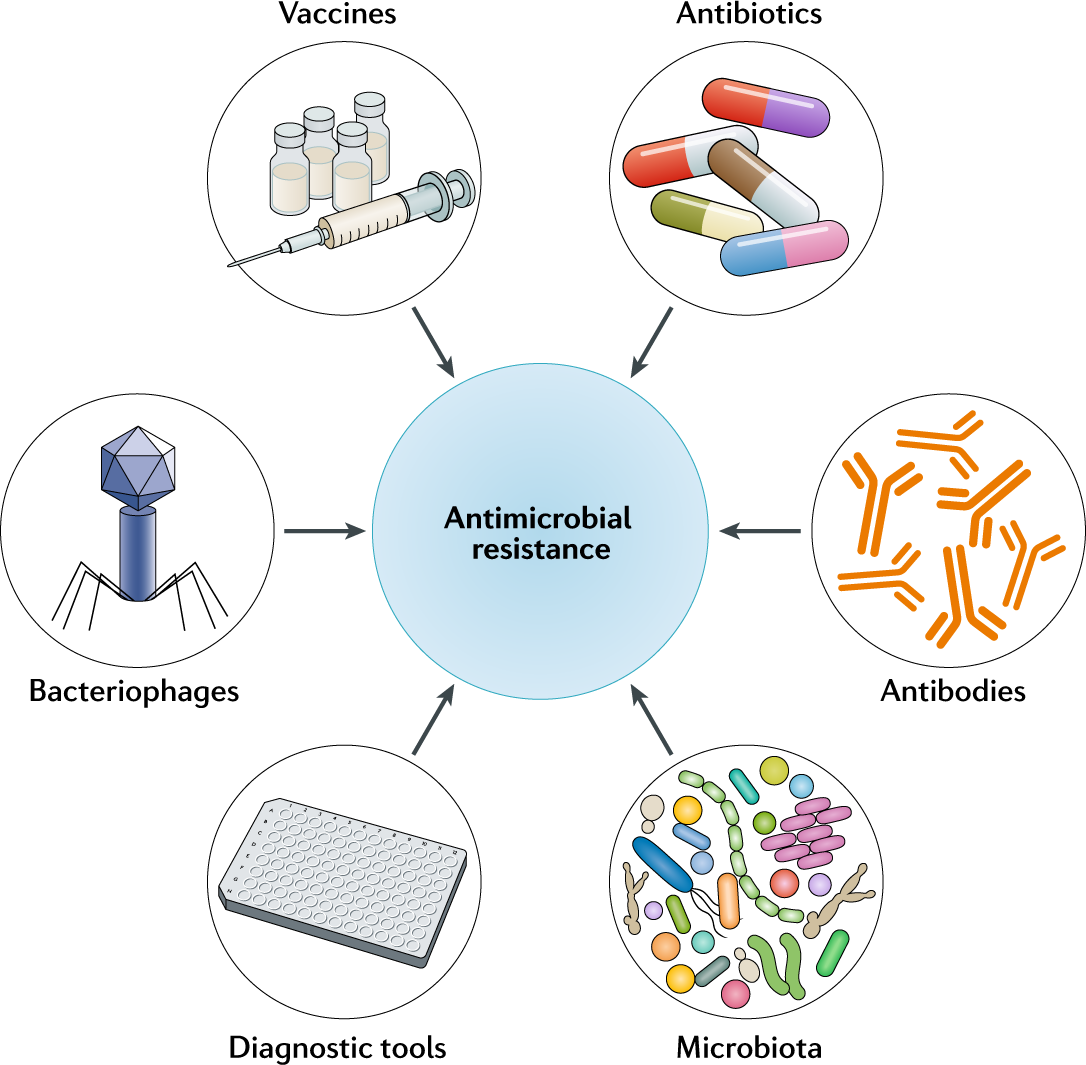
One of the pressing issues in modern medicine is the rise of antibiotic resistance, a phenomenon where bacteria develop the ability to survive exposure to antibiotics that were previously effective against them. This poses a significant threat to public health, as treating infections becomes increasingly challenging and costly.
Factors Contributing to Antibiotic Resistance
Antibiotic resistance can be attributed to several factors, including:
- Overprescription of antibiotics
- Improper use of antibiotics
- Incomplete courses of antibiotic treatment
- Use of antibiotics in livestock for growth promotion
Impact of Antibiotic Resistance on Superinfections
Antibiotic resistance plays a critical role in the development of superinfections. Initially, the overuse and misuse of antibiotics create an environment where bacteria evolve and become resistant to these medications. This resistance can lead to the emergence of superinfections, which are infections caused by bacteria that are resistant to multiple antibiotics.
Understanding Superinfections
Superinfections are a phenomenon where a new infection occurs during the course of an existing one, leading to complications and prolonged treatment. It is crucial to understand what event triggers the development of a superinfection to effectively manage patient care and outcomes.
Causes of Superinfections
Superinfections can be sparked by various factors, including the inappropriate use of antibiotics, compromised immune system, prolonged hospital stays, and invasive medical procedures. These predisposing factors create an environment conducive to the emergence of secondary infections.
Additionally, the overuse or misuse of antibiotics contributes to the development of drug-resistant strains of bacteria and fungi, increasing the risk of superinfections.
Prevention and Management Strategies
To prevent superinfections, healthcare providers must adhere to proper infection control practices, judicious antibiotic prescribing, and vigilant monitoring of patients at risk. It is essential to educate both healthcare professionals and patients on the importance of antimicrobial stewardship to combat the rise of superinfections.
- Hand hygiene: Regular handwashing can significantly reduce the spread of infections in healthcare settings.
- Monitoring antibiotic use: Surveillance and restriction of antibiotic use can help prevent the development of resistant bacteria.
- Early detection: Prompt recognition of superinfections allows for timely intervention and treatment modification.
Factors Fueling Superinfection Development
Superinfections are typically triggered by a combination of factors that create an ideal environment for multiple pathogens to thrive simultaneously. Understanding these factors is crucial in managing and preventing the development of superinfections.
1. Prolonged Antibiotic Use
One of the primary factors contributing to superinfection development is prolonged antibiotic use. When antibiotics are overprescribed or used incorrectly, they can disrupt the natural balance of microorganisms in the body, leading to the proliferation of drug-resistant pathogens.
2. Compromised Immune System
Individuals with a compromised immune system are particularly vulnerable to superinfections. Conditions such as HIV/AIDS, cancer, and autoimmune disorders can weaken the body’s defenses, making it easier for multiple pathogens to take hold and cause infections.
3. Healthcare Settings
Healthcare settings play a significant role in superinfection transmission. Hospitals and long-term care facilities are breeding grounds for drug-resistant bacteria and other pathogens due to close proximity among patients, frequent use of antibiotics, and invasive medical procedures.
Exploring Triggering Events
Understanding what event triggers the development of a superinfection is crucial in combating the growing concern of antibiotic resistance. Superinfections occur when a patient already infected with one pathogen contracts a secondary infection due to various triggering events.
The Role of Antibiotic Misuse
One significant triggering event is the misuse of antibiotics, leading to the emergence of resistant strains of bacteria. This results in a weakened immune system making the patient more susceptible to superinfections.
Immunocompromised Patients
Immunocompromised patients, such as those undergoing chemotherapy or organ transplant recipients, are at a higher risk of developing superinfections due to their weakened immune systems.
- Chemotherapy patients
- Organ transplant recipients
- HIV/AIDS patients
Recognition and Management Strategies
When considering what event triggers the development of a superinfection, it is vital to focus on recognition and management strategies to combat this issue effectively. Healthcare professionals need to be adept at identifying the signs and symptoms of superinfections promptly.
Early Detection Methods
Early recognition can significantly impact the outcome of superinfections. Utilizing advanced diagnostic tools such as PCR testing can aid in the swift identification of pathogens responsible for the superinfection.
Increased Surveillance Protocols
Ramping up surveillance mechanisms in healthcare settings can play a crucial role in early detection. Implementing real-time monitoring systems can help in identifying trends and patterns that may indicate a potential superinfection outbreak.
Management Approaches
Managing superinfections requires a multifaceted approach involving antimicrobial stewardship programs and infection control measures.
Antimicrobial Stewardship
Adhering to antibiotic guidelines and employing tactics such as de-escalation therapy can aid in preventing the development of superinfections due to antibiotic resistance.
Infection Control Measures
Implementing robust infection control protocols, including proper hand hygiene practices and environmental cleaning, is crucial in preventing the spread of superinfections within healthcare facilities.
Frequently Asked Questions
-
- What is a superinfection?
- A superinfection is an additional infection that occurs in a person who is already infected with another pathogen or microorganism.
-
- What event triggers the development of a superinfection?
- The development of a superinfection is typically triggered by factors such as weakened immune system, prolonged antibiotic usage, or exposure to multiple pathogens.
-
- How does a weakened immune system contribute to a superinfection?
- A weakened immune system is more vulnerable to secondary infections, making it easier for new pathogens to take hold and cause a superinfection.
-
- Can prolonged antibiotic usage lead to a superinfection?
- Yes, prolonged antibiotic usage can disrupt the normal balance of microorganisms in the body, potentially leading to the development of a superinfection.
-
- Are there specific risk factors that increase the likelihood of a superinfection?
- Yes, risk factors such as hospitalization, invasive medical procedures, and immunosuppressive medications can increase the likelihood of developing a superinfection.
Unraveling Superinfections: The Triggering Event
As we reach the conclusion of our exploration into what event sparks the development of a superinfection, it becomes evident that various factors can set the stage for these complex medical scenarios. From antibiotic overuse to compromised immune systems, the susceptibility to superinfections is a real concern in healthcare settings. Understanding the delicate balance between host and pathogen is crucial in managing and preventing superinfections. By recognizing the significance of proper hygiene practices, vigilant monitoring, and appropriate antibiotic stewardship, we can strive towards minimizing the risks of superinfections and promoting better patient outcomes. Remember, knowledge is key in combating these challenging healthcare dilemmas. Stay informed, stay vigilant!

