Have you ever wondered about the intricate sequence of events that pave the way for an infection to take hold in the human body? Understanding the pathway that leads to an infection is crucial in order to prevent and manage such health threats effectively. In this blog, we will delve deep into the underlying mechanisms and factors that set the stage for infections to develop. By unraveling this mystery, we can gain valuable insights into the vulnerabilities of our immune system, the role of pathogens, and the environmental factors that contribute to the initiation of infections. Join us on this enlightening journey to explore the what, how, and why behind the sequence of events that lead to an infection.
Introduction to Infections
Infections are a common occurrence caused by the invasion of pathogens into the body, triggering a response from the immune system. Understanding what sequence of events lead to an infection is crucial in preventing and treating them effectively.
Types of Infections
There are various types of infections, including bacterial, viral, fungal, and parasitic infections. Each type has its own characteristics and modes of transmission.
Transmission of Infections
Infections can be transmitted through various means such as direct contact, respiratory droplets, contaminated food or water, and insect bites. Proper hygiene practices and immunizations play a critical role in preventing the spread of infections.
The Basics of Pathogen Transmission
Understanding how pathogens are transmitted is essential in comprehending what sequence of events leads to an infection. Pathogen transmission can occur through various routes, including direct contact, indirect contact, respiratory droplets, and vectors.
Direct Contact Transmission
Direct contact transmission involves physical contact between an infected individual and a susceptible person. This can occur through activities such as touching, kissing, or sexual intercourse.
Indirect Contact Transmission
Indirect contact transmission occurs when a susceptible individual comes into contact with contaminated surfaces or objects. Pathogens can survive on surfaces for extended periods, increasing the risk of transmission.
- Regular handwashing is crucial in preventing indirect contact transmission.
- Disinfecting commonly touched surfaces can help reduce the spread of pathogens.
Respiratory Droplet Transmission
Respiratory droplet transmission occurs when an infected individual exhales, coughs, or sneezes, releasing droplets containing pathogens into the air. These droplets can be inhaled by nearby individuals, leading to potential infection.
Vector-Borne Transmission
Vector-borne transmission involves the transfer of pathogens from an infected host to a susceptible individual through a vector, such as mosquitoes or ticks. These vectors act as carriers of the disease, facilitating its spread.
The Role of Host Susceptibility
Host susceptibility plays a crucial role in determining the likelihood of an infection taking hold within an individual. The genetic makeup and overall health status of a host can significantly influence their vulnerability to pathogens and the subsequent development of an infection.
Genetic Factors
Genetic predispositions can impact how the immune system responds to invading pathogens, making certain individuals more susceptible to infections. Variations in genes related to immune function can either enhance or compromise the body’s ability to combat pathogens.
Individuals with genetic mutations affecting immune responses may exhibit increased susceptibility to specific infections, highlighting the intricate interplay between genetics and infection susceptibility.
Health Status
Host susceptibility is also influenced by overall health status, which encompasses factors such as nutrition, underlying medical conditions, and lifestyle choices. Poor nutrition or pre-existing health conditions can weaken the immune system, making the host more prone to infections.
Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and adequate rest, can bolster the immune system and reduce the risk of infections. Additionally, vaccination against preventable diseases can further enhance host immunity.
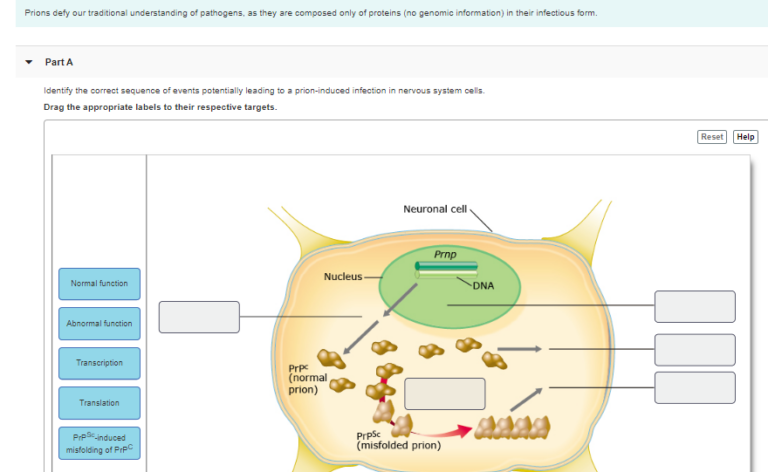
Initiation of Infection: Entry and Adhesion
When exploring what sequence of events lead to an infection, understanding the initiation of infection is crucial. The process typically begins with the entry of a pathogen into the host’s body. This entry can occur through various routes, such as inhalation, ingestion, or direct contact with the skin.
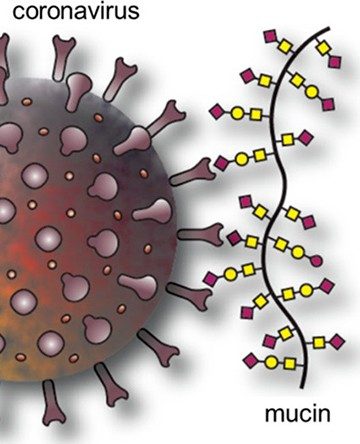
Adhesion to Host Cells
Once the pathogen enters the body, it needs to adhere to host cells to establish an infection. Adhesion is facilitated by specific molecules on the surface of the pathogen that interact with receptors on the host cell. This binding initiates a series of events that allow the pathogen to invade and replicate within the host.
Establishment and Multiplication of Pathogens
Pathogens are microorganisms that can cause disease in a host organism. The process of infection begins with the establishment and multiplication of these pathogens within the host’s body. Understanding this sequence of events is crucial in unraveling the mystery of how infections occur.
Adherence and Colonization
Once a pathogen enters the host, it must first adhere to the host’s cells to establish an infection. Adherence is facilitated by specific surface molecules on the pathogen that bind to receptors on the host cell, allowing the pathogen to colonize and multiply.
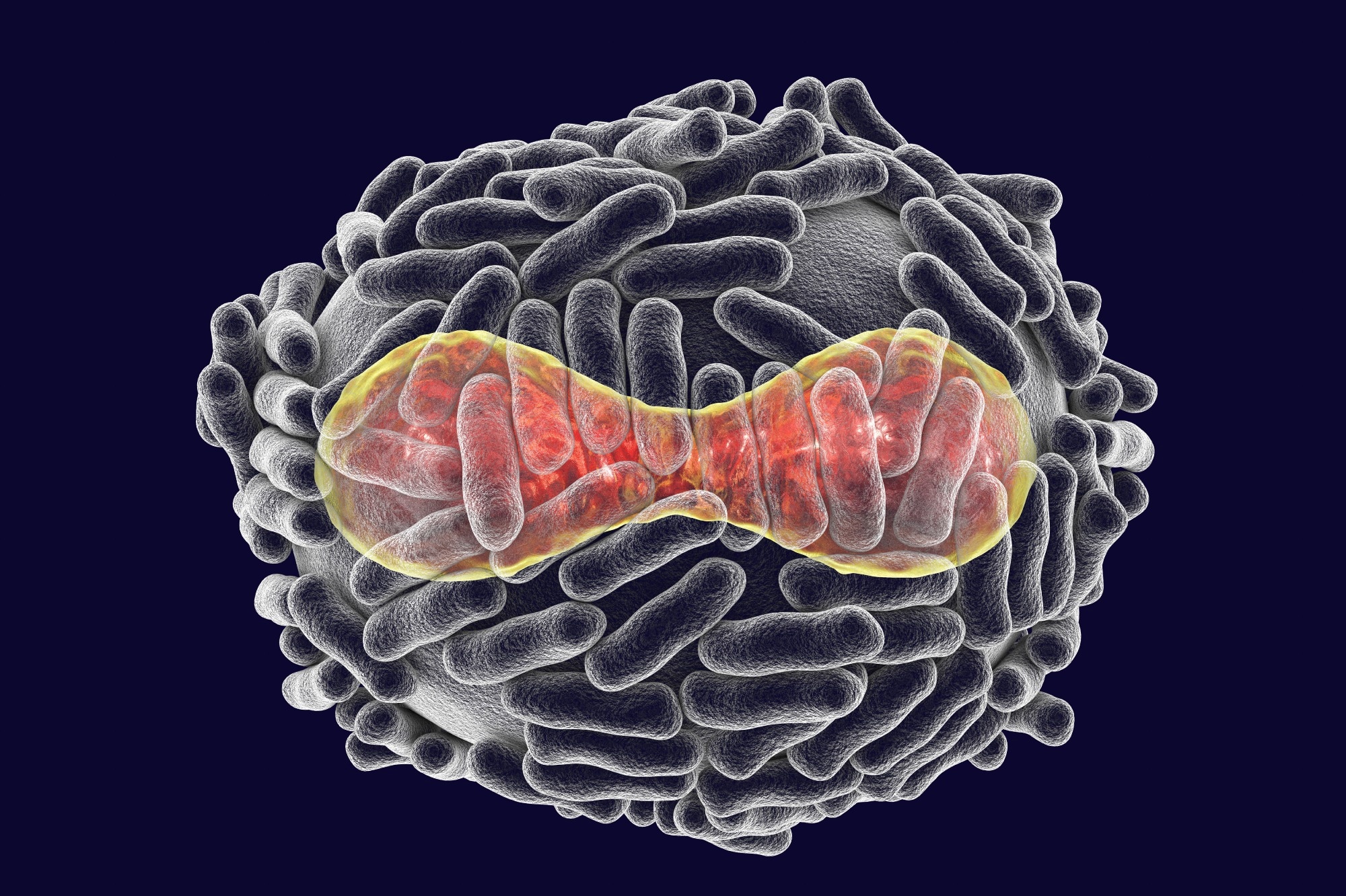
During colonization, the pathogen forms a biofilm or establishes a niche within the host where it can evade the immune system and proliferate.
Evading the Immune System
Pathogens have developed various mechanisms to evade the host’s immune system. This includes disguising themselves to avoid detection, releasing toxins to impair immune cell function, or hiding within host cells to escape immune surveillance.
- Some pathogens can modulate host immune response to create an environment favorable for their survival.
- Others suppress immune system activation to prevent clearance by immune cells.
Evading the Immune System
When examining what sequence of events lead to an infection, understanding how pathogens evade the immune system is crucial. Pathogens have evolved various strategies to outsmart the body’s defense mechanisms, enabling them to establish infections.
Camouflage Techniques
One common evasion tactic is the use of molecular mimicry. Pathogens disguise themselves by mimicking host molecules, making it difficult for the immune system to distinguish between self and non-self. This allows the pathogen to evade detection and attack.
Antigenic Variation
Another strategy employed by pathogens is antigenic variation. By constantly changing the surface proteins or antigens, pathogens can stay one step ahead of the immune response, as the antibodies produced against the previous antigens are rendered ineffective against the new ones.
This continuous antigenic variation poses a significant challenge for the immune system to mount an effective defense, allowing the pathogen to persist and cause infection.
Immune Suppression
Some pathogens have developed mechanisms to suppress the immune system. They can inhibit the activation of immune cells, prevent the release of pro-inflammatory signals, or induce regulatory immune responses that dampen the overall immune reaction.
By downregulating the immune response, pathogens can avoid detection and clearance, leading to persistent infections.
Spread and Transmission of Infection
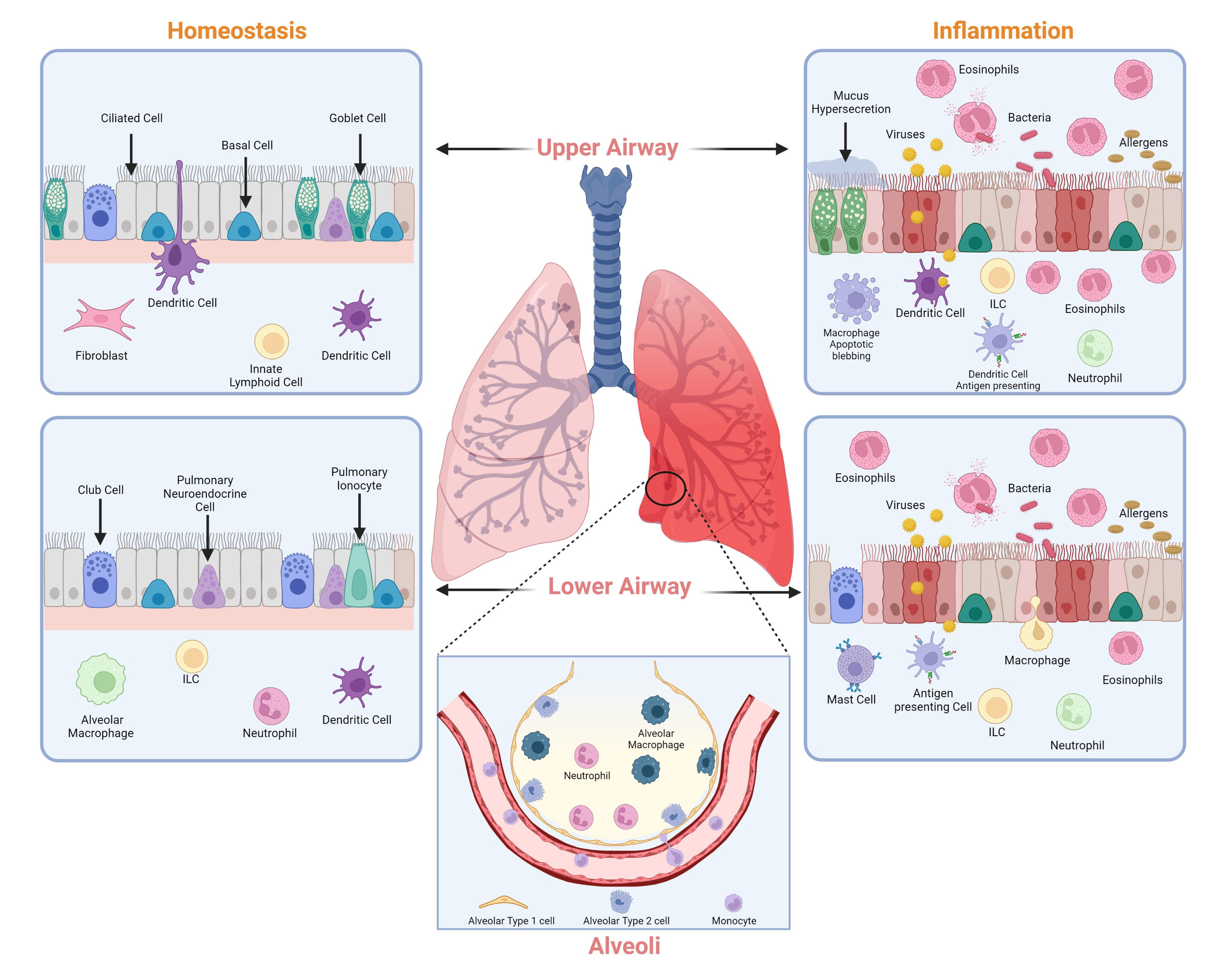
Understanding the spread and transmission of infections is crucial in preventing outbreaks. Infections can be transmitted through various means, including direct contact, indirect contact, respiratory droplets, and airborne particles.
Direct Contact
Direct contact is one of the most common ways infections spread. This can occur through touching an infected person, kissing, or sexual contact. It is essential to practice good hand hygiene to prevent the spread of infections.
Indirect Contact
Indirect contact transmission involves touching surfaces or objects contaminated with infectious agents. Regularly disinfecting commonly touched surfaces like doorknobs, light switches, and phones can help prevent the spread of infections.
Respiratory Droplets
Respiratory droplets are tiny liquid particles expelled when an infected person talks, coughs, or sneezes. These droplets can land in the mouths or noses of people nearby, leading to infection. Wearing masks and practicing social distancing can reduce the transmission of respiratory infections.
Airborne Transmission
Airborne transmission occurs when infectious agents are present in droplet nuclei that remain suspended in the air for more extended periods. Ventilating indoor spaces and using air purifiers can help minimize the risk of airborne infections.
Factors Influencing Infection Development
Understanding the sequence of events that lead to an infection is crucial in combatting and preventing its spread. Several factors impact the development of infections, ranging from environmental conditions to host immunity.
Environmental Factors
Environmental factors play a significant role in the development of infections. The presence of pathogens in the environment, such as bacteria or viruses, increases the risk of infections. Proper sanitation measures year 2022 are essential to prevent the spread of infectious agents.
Host Immunity
Host immunity is another critical factor influencing infection development. A strong immune system can effectively fight off invading pathogens, reducing the likelihood of infection. Regular exercise and a balanced diet year 2022 can boost immunity and reduce infection risk.
Frequently Asked Questions
-
- What are the common sequence of events that lead to an infection?
- The common sequence of events that lead to an infection typically involve introduction of a pathogen, colonization, invasion, and multiplication within the host organism.
-
- How does the body respond to an infection?
- The body responds to an infection by activating the immune system, which includes both innate (immediate) and adaptive (specific) immune responses to combat the pathogen.
-
- What role do pathogens play in the process of infection?
- Pathogens are disease-causing agents that play a crucial role in the process of infection by entering the host, evading the immune response, and causing damage to host tissues.
-
- Can infections be prevented?
- Infections can often be prevented through practices such as good hygiene, vaccination, maintaining a healthy lifestyle, and avoiding exposure to known pathogens.
-
- What are the common signs and symptoms of an infection?
- Common signs and symptoms of an infection include fever, fatigue, inflammation, redness, swelling, pain, and in severe cases, organ dysfunction.
Final Thoughts
Understanding what sequence of events leads to an infection is crucial in preventing and treating various illnesses. From initial exposure to a pathogen to the invasion of the body, each step plays a vital role in the development of an infection. The interplay between the pathogen’s virulence factors and the host’s immune response determines the outcome. By unraveling this mystery, healthcare professionals can devise effective strategies for infection control and management.
Remember, maintaining good hygiene practices, getting vaccinated, and seeking prompt medical attention are key steps in reducing the risk of infections. Stay informed, stay safe, and prioritize your health!